Understanding Nutritional Ketosis
Nutritional ketosis is a metabolic state where the body uses fat as its primary energy source instead of carbohydrates. This state is achieved through a ketogenic diet, which is high in fat and very low in carbohydrates. The ketogenic diet prompts the liver to convert fat into ketone bodies, including β-hydroxybutyrate (BHB) and acetoacetate (AcAc), which can be used for energy by various tissues in the body, including the brain and muscles.
When the body enters ketosis, it effectively shifts its fuel source from glucose to fat. This shift occurs because the low carbohydrate intake reduces blood glucose levels, leading to lower insulin levels. As insulin levels drop, the body begins to break down stored fat into fatty acids and glycerol. The liver then converts these fatty acids into ketone bodies through a process called ketogenesis.
Ketone bodies are a more efficient energy source during critical illness when the body’s ability to utilize glucose is impaired. They provide a steady supply of energy without the need for glucose and help maintain cellular functions even under stress. This alternative energy pathway is particularly beneficial in situations where inflammation and oxidative stress are prevalent, as it helps reduce the detrimental effects of these conditions on the body’s cells.

The ketogenic diet mimics the metabolic effects of fasting without significant caloric restriction. This makes it a practical approach for maintaining nutritional status while achieving the benefits of ketosis.
By sustaining a state of nutritional ketosis, critically ill patients can potentially experience improved energy production, reduced inflammation, and enhanced recovery outcomes.
Understanding the mechanisms of nutritional ketosis lays the foundation for exploring its specific benefits in critical illness, which we will explore in the following sections.
The ketogenic diet mimics the metabolic effects of fasting without significant caloric restriction.
By sustaining a state of nutritional ketosis, critically ill patients can potentially experience improved energy production, reduced inflammation, and enhanced recovery outcomes.
Bioenergetic Benefits of the Keto Diet for Critical Illness
The keto diet offers significant bioenergetic benefits for critical illness. During severe illness, the body’s ability to use glucose for energy often fails. This failure leads to energy shortages that can worsen the condition. Ketone bodies, produced during ketosis, provide an alternative energy source that can bypass these metabolic blocks.
Ketone bodies, such as β-hydroxybutyrate (BHB) and acetoacetate (AcAc), are created from fat in the liver. They serve as a stable and efficient energy source for vital organs and tissues, including the brain and muscles.
The study notes, “Ketone bodies can be a useful energy resource for tissue inflammation and hypoxia,” highlighting their potential to sustain energy production when traditional pathways are impaired.
In critical illness, the metabolic shift to ketosis allows the body to maintain energy levels despite impaired glucose utilization. This shift helps to stabilize patients and improve their overall condition. The ketogenic diet prompts this metabolic change by reducing carbohydrate intake and increasing fat consumption, forcing the body to rely on fat-derived ketones for energy.

This bioenergetic benefit is crucial because it supports cellular functions and prevents energy deficits that can exacerbate critical conditions. By providing a continuous energy supply, ketone bodies help maintain cellular health and function, which is vital for recovery and stabilization in critically ill patients.
The keto diet’s ability to offer an alternative energy source during metabolic crises represents a significant advantage in managing critical illnesses. This metabolic flexibility can help improve patient outcomes by ensuring that energy production continues even when the body cannot use glucose effectively.
The keto diet’s bioenergetic benefit supports cellular functions and prevents energy deficits that can exacerbate critical conditions.
This represents a significant advantage in managing critical illnesses.
Anti-Inflammatory Effects
The keto diet provides significant anti-inflammatory benefits for critical illness. Inflammation plays a central role in many severe health conditions, making its management crucial. Ketone bodies, produced during ketosis, possess potent anti-inflammatory properties.
Ketones inhibit inflammasomes, which are protein complexes that trigger inflammation. By preventing the release of pro-inflammatory cytokines, ketones reduce overall inflammation.
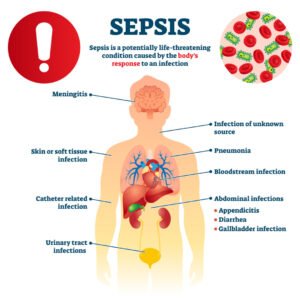
The study highlights this effect: “Ketones inhibit inflammasomes, preventing the secretion of pro-inflammatory cytokines.” This action is particularly beneficial in conditions like sepsis and acute respiratory distress syndrome (ARDS), where inflammation is a key factor.
Reducing inflammation helps stabilize patients and prevents further complications. In critical illnesses, excessive inflammation can damage tissues and organs, worsening the patient’s condition. The anti-inflammatory properties of ketones help mitigate this damage, promoting better outcomes.
In addition, ketones can regulate the immune response. They decrease the activity of certain immune cells that contribute to chronic inflammation. This regulation ensures that the immune response remains balanced, reducing the risk of prolonged or excessive inflammation.
Ketones inhibit inflammasomes, which are protein complexes that trigger inflammation, which helps to stabilize patients and prevent further complications.
This action is particularly beneficial in conditions like sepsis and acute respiratory distress syndrome (ARDS), where inflammation is a key factor.
The ketogenic diet, by promoting the production of anti-inflammatory ketones, offers a valuable tool in managing critical illnesses. It helps control inflammation, which is essential for patient recovery and stabilization. By integrating this dietary approach, healthcare providers can enhance treatment strategies for critically ill patients.
The anti-inflammatory effects of nutritional ketosis underscore its potential as a therapeutic approach. These benefits contribute significantly to improving patient outcomes and managing critical illness effectively.
Antioxidant Properties of Nutritional Ketosis
The keto diet also provides antioxidant benefits, which are crucial for managing critical illness. Oxidative stress, characterized by an imbalance between free radicals and antioxidants, can worsen many severe health conditions. Ketone bodies, produced during ketosis, help counteract oxidative stress and protect cells from damage.
Ketones enhance mitochondrial biogenesis and control mitophagy, processes that reduce oxidative damage. The study explains, “Ketones control mitophagy and increase mitochondrial biogenesis, providing beneficial antioxidant effects and preserving cellular energy.” This means ketones help create new mitochondria, the energy powerhouses of cells, and remove damaged ones, reducing oxidative stress.
Reducing oxidative stress is essential in critical illness, as it can damage tissues and impair organ function. By acting as antioxidants, ketones help maintain cellular health and function. This protective effect supports better outcomes in critically ill patients by preventing further deterioration.

Ketone bodies like β-hydroxybutyrate (BHB) and acetoacetate (AcAc) also work directly as antioxidants. They scavenge free radicals, molecules that can cause cellular damage. This direct antioxidant action adds another layer of protection, helping to stabilize patients and promote recovery.
The ketogenic diet mimics fasting by significantly lowering carbohydrate intake and increasing fat consumption. This dietary shift promotes the production of ketones, ensuring a steady supply of these beneficial molecules. As a result, patients experience reduced oxidative stress and improved cellular function, contributing to better overall health outcomes.
Ketones enhance mitochondrial biogenesis and control mitophagy, processes that reduce oxidative damage.
As a result, patients experience reduced oxidative stress and improved cellular function, contributing to better overall health outcomes.
References
- Nutritional Ketosis as a Therapeutic Approach in Critical Illness: A Systematic Review. Cureus
- Is there a role for ketones as alternative fuel in critical illness? Current Opinion in Critical Care
- A pilot study of alternative substrates in the critically Ill subject using a ketogenic feed. Nature Communications
- Ketogenic diet benefits in critically ill patients with sepsis. Nature Reviews Nephrology
Keto PowerFlax Baking Mix: Keto & So Much More!

- Commercial Bakeries: you can easily produce delicious flax-based keto-friendly products which are clean label, high protein, high fiber and vegan
- Works with your current equipment and baking processes
- Recipes provided on all bulk orders, with ongoing customer support
- Worldwide shipping
- Get in touch with us today!